Cancers that become resistant to an important class of drugs might be made vulnerable by tweaking the immune system, a team led by UCSD researcher Napolene Ferrara has found.
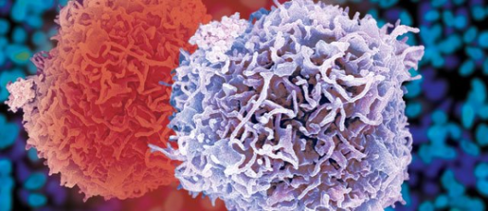
Cancers that become resistant to an important class of drugs might be made vulnerable by tweaking the immune system, a team led by UCSD researcher Napolene Ferrara has found.Growing tumors induce the formation of blood vessels, which supply nutrition that tumors need to grow. Drugs that block this process, called angiogenesis, include the popular drugs Avastin, Gleevec and Sutent. However, cancers usually develop resistance to these drugs and resume growing. A false-color scanning electron micrograph, depicting a pair of white blood cells or leukocytes. These cells express interleukin-17, implicated in promoting cancer drug resistance. A chemical called interleukin-17 involved in the immune response to infection promotes resistance to the drugs in lymphoma, lung and colon cancers, according to a study published Sunday in Nature Medicine. Ferrara was the papers senior author. Moreover, drugs already in clinical testing for other diseases block interleukin-17, Ferrara said. This means it might be possible to use these drugs to make these resistant cancers once again vulnerable to the antiangiogenesis drugs. Ferrara said it should be fairly easy to develop tests for biomarkers to spot tumors that have developed IL-17-based resistance. Patients with these biomarkers could then be given drugs to block that chemical, once again making the tumors vulnerable to drugs like Avastin. Angiogenesis-blocking drugs arose out of research by the late Judah Folkman, who noted that cancers require a blood supply to grow. Normally, blood vessels remain in a steady state condition in the body, neither growing nor shrinking. So when cancers grow, they must somehow signal the body to produce more blood vessels to feed them. A number of other researchers, including Ferrara, followed that line of reasoning to develop drugs to block angiogenesis. A chemical called vascular endothelial growth factor, or VEGF, promotes the growth of blood vessels. Drugs like Avastin stop VEGF from working. Ferrara played a key role in identifying the gene that makes VEGF, which led to Avastin and other drugs in its class. Avastin is a monoclonal antibody developed by Genentech that binds to VEGF, making it ineffective. So when cancers develop resistance to drugs like Avastin, something is presumably happening to get around this effect. The study found that interleukin 17 lies at the center of a complex network of molecules that promote angiogenesis independent of VEGF. Blocking IL-17 disrupts this network, once again making the cancer sensitive to VEGF-blocking drugs. To establish the role of IL-17, the researchers found evidence from multiple sources, all of which found that the chemical is central to developing resistance to the angiogenesis drugs. First, immune cells that secrete the chemical are found in tumors resistant to the angiogenesis drugs. The greater their number, the worse the prognosis for therapy. Resistant tumors were also transplanted into mice. They were treated with the angiogenesis drugs, in combination with an antibody that blocks IL-17, and with a control antibody that did not block IL-17. The combo treatment that blocked IL-17 reduced tumor growth by half, compared with the control. In addition, resistant tumors were transplanted into knockout mice in which the gene to make IL-17 was disabled. The mice were dosed with the cancer drugs, and compared with control mice that retained the ability to make IL-17. Tumor growth was reduced by nearly 80 percent in the knockout mice, compared to control mice.